Cervical canal
| Cervical canal | |
|---|---|
 | |
 | |
| Details | |
| Synonym | Canal of the cervix, endocervical canal, cervical canal of uterus, cavity of cervix |
| Identifiers | |
| Latin | canalis cervicis uteri |
| TA | A09.1.03.018 |
| FMA | 86485 |
| Anatomical terminology | |
The cervical canal is the flattened canal going through the cervix. The cervix is the lower part of the uterus.
Anatomy[change | change source]
The cervical canal is a tube that connects with the uterine cavity through the internal os with the vagina through the external os. The internal os is smaller than the external os. The external os is a small, circular opening on the rounded end of the cervix. The external os opens into the vagina. The cervical cavity is located at the top of the vagina. The external os is surrounded by two lips, an anterior lip and a posterior lip. The anterior lip is shorter and thicker. Both lips are touching the vaginal wall. Before pregnancy, the external os has a rounded shape. After pregnancy the os changes shape.
Type 1: Completely ectocervical (common under hormonal influence).
Type 2: Endocervical component but fully visible (common before puberty).
Type 3: Endocervical component, not fully visible (common after menopause).
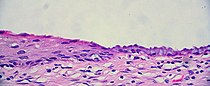
The cervical canal is lined by a tissue called the "endocervical mucosa". This consists of a single layer of mucinous columnar epithelium. After menopause the tissue goes through changes.[2]
Pathology[change | change source]

The endocervical mucosa is one place tissue from where cervical cancer (adenocarcinoma) can grow. Endocervical adenocarcinoma, like another cervical cancer (squamous cell carcinoma), often grows from human papilloma virus infection.[3]
Related pages[change | change source]
References[change | change source]
- ↑ International Federation for Cervical Pathology and Colposcopy (IFCPC) classification. References:
-"Transformation zone (TZ) and cervical excision types". Royal College of Pathologists of Australasia.
- Jordan, J.; Arbyn, M.; Martin-Hirsch, P.; Schenck, U.; Baldauf, J-J.; Da Silva, D.; Anttila, A.; Nieminen, P.; Prendiville, W. (2008). "European guidelines for quality assurance in cervical cancer screening: recommendations for clinical management of abnormal cervical cytology, part 1". Cytopathology. 19 (6): 342–354. doi:10.1111/j.1365-2303.2008.00623.x. ISSN 0956-5507. PMID 19040546. S2CID 16462929. - ↑ Beckmann, Charles R B A; Herbert, William; Laube, Douglas; Ling, Frank; Smith, Roger (March 2013). Obstetrics and Gynecology (7th ed.). pp. 408–11. ISBN 9781451144314.
- ↑ Yeh, IT.; LiVolsi, VA.; Noumoff, JS. (Mar 1991). "Endocervical carcinoma". Pathol Res Pract. 187 (2–3): 129–44. doi:10.1016/S0344-0338(11)80763-6. PMID 2067992.