Dengue fever
The English used in this article or section may not be easy for everybody to understand. (February 2012) |
| Dengue fever | |
|---|---|
| Classification and external resources | |
 The typical rash seen in dengue fever | |
| ICD-10 | A90. |
| ICD-9 | 061 |
| DiseasesDB | 3564 |
| MedlinePlus | 001374 |
| eMedicine | med/528 |
| MeSH | C02.782.417.214 |
Dengue fever is an infection caused by the dengue virus. Mosquitoes transmit (or spread) the dengue virus. Dengue fever is also known as "break-bone fever" or "bone-break fever", because it can cause people to have pain so bad that they feel like their bones are breaking. Some of the symptoms of dengue fever are fever; headache; a skin rash that looks like measles; and pain in the muscles and joints. In a few people, dengue fever can turn into one of two forms that are life-threatening. The first is dengue hemorrhagic fever, which causes bleeding, leaking blood vessels (tubes which carry blood), and low levels of blood platelets (which cause the blood to clot). The second is dengue shock syndrome, which causes dangerously low blood pressure.
There are four different types of the dengue virus. Once a person has been infected with one type of the virus, he usually is protected from that type for the rest of his life. However, he will only be protected against the other three types of the virus for a short time. If he later gets one of those three types of the virus, he will be more likely to have serious problems.
There is no vaccine that works to keep people from getting the dengue virus. There are a few things that can be done to prevent people from getting dengue fever. People can protect themselves against mosquitoes and limit the number of bites they get. Scientists also suggest making mosquito habitats smaller and reducing the number of mosquitoes that exist. Once a person has dengue fever, he usually can recover just by drinking enough fluids, as long as his disease is mild or moderate. If the person has a more severe case, he may need intravenous fluids (fluids given into a vein, using a needle and tubing), or blood transfusions (being given blood from another person).
Since the 1960s, many more people have been getting dengue fever. The disease has become a worldwide problem since the Second World War. It is common in more than 110 countries. Every year, around 50–100 million people get dengue fever.
People are working on a vaccine and medication to treat the virus directly. People also do many different things to try to get rid of mosquitoes.
The first descriptions of dengue fever were written in 1779. Early in the 20th century, scientists learned that the disease is caused by the dengue virus, and that it is transmitted (or spread) by mosquitoes.
Signs and symptoms
About 80% of people (or 8 out of every 10) who are infected with the dengue virus have no symptoms, or have only mild symptoms (like a basic fever).[1][2][3] About 5% of infected people (or 5 out of every 100) become more seriously ill. In a small number of these people, the disease is life-threatening.[1][3] Symptoms appear between 3 and 14 days after a person is exposed to the dengue virus. Most often, symptoms appear after 4 to 7 days.[4] So if a person returns from an area where dengue is common, and gets a fever or other symptoms more than 14 days after he returned, he probably does not have dengue.[5]
Often, when children have dengue fever, their symptoms are the same as the common cold or gastroenteritis (or stomach flu; for example, vomiting and diarrhea).[6] However, children are more likely to have severe problems from dengue fever.[5]
Clinical course
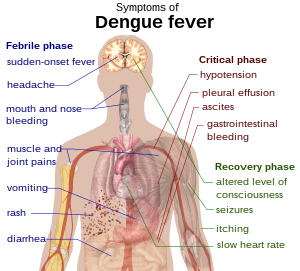
The classic symptoms of dengue fever are a fever that begins suddenly; a headache (usually behind the eyes); a rash; and muscle and joint pains. The disease's nickname, "break-bone fever" describes how severe this pain can be.[1][7] Dengue fever happens in three stages: febrile, critical, and recovery.[8]
In the febrile stage, a person usually has a high fever. ("Febrile" means that a person has a fever.) The fever is often over 40 degrees Celsius (104 degrees Fahrenheit). The person may also have general pains and a headache. The febrile stage usually lasts 2 to 7 days.[7][8] At this stage, about 50 to 80% of people who have symptoms get a rash.[7][9] On the first or second day, the rash can look like flushed (red) skin. Later in the illness (on days 4 to 7), the rash can look like measles.[9][10] Small red spots (petechiae) can appear on the skin. These spots do not disappear when the skin is pressed. These red spots are caused by broken capillaries. [8] The person may also have mild bleeding from the mucous membranes of the mouth and nose.[5][7] The fever itself tends to break (get better) and then return for one or two days. However, this pattern happens differently in different people.[10][11]
In some people, the disease goes into a critical phase after the high fever is gone. The critical phase usually lasts 1 to 2 days.[8] During this phase, fluid can build up in the chest and abdomen. This happens because small blood vessels are leaking. The fluid builds up, and it no longer circulates around the body. This means that the vital (most important) organs do not get as much blood as usual.[8] Because of this, the organs do not work normally. The person can also have severe bleeding (usually from the gastrointestinal tract.)[5][8]
Less than 5% of people with dengue get circulatory shock, dengue shock syndrome, and dengue hemorrhagic fever.[5] If a person has had another type of dengue before ("secondary infection"), they are more likely to have these serious problems.[5][12]
In the recovery stage, the fluid that leaked out of the blood vessels is taken back up into the bloodstream.[8] The recovery stage usually lasts 2 to 3 days.[5] The person often gets much better during this stage. However, they can have severe itching and a slow heart rate.[5][8] During this stage, the person can go into a fluid overload state (where too much fluid is taken back up). If it affects the brain, it can cause seizures or an altered level of consciousness (where the person's thinking, awareness, and behavior can be different than usual).[5]
Associated problems
Every once in a while, dengue can affect other systems in the body.[8] A person can have symptoms alone, or along with the classic dengue symptoms.[6] A decreased level of consciousness occurs in 0.5–6% of severe cases. This can happen when the dengue virus causes an infection in the brain. It can also happen when vital organs, like the liver, are not working correctly.[6][11]
Other neurological disorders (disorders affecting the brain and nerves) have been reported in people who have dengue fever. For example, dengue can cause transverse myelitis and Guillain-Barré syndrome.[6] Although this almost never happens, dengue can also cause infection of the heart and acute liver failure.[5][8]
Cause
Dengue fever is caused by the dengue virus. In the scientific system that names and classifies viruses, the dengue virus is part of the family Flaviviridae and the genus Flavivirus. Other viruses also belong to the same family and cause disease in humans. For example, yellow fever virus, West Nile virus, St. Louis encephalitis virus, Japanese encephalitis virus, tick-borne encephalitis virus, Kyasanur forest disease virus, and Omsk hemorrhagic fever virus all belong to the family Flaviviridae..[11] Most of these viruses are spread by mosquitoes or ticks.[11]
Transmission

Dengue virus is transmitted (or spread) mostly by Aedes mosquitoes, especially the Aedes aegypti type of mosquito.[2] These mosquitoes usually live between the latitudes of 35° North and 35° South, below an elevation of 1000 m.[2] They bite mostly during the day.[13] A single bite can infect a person.[14]
Sometimes, mosquitoes can also get dengue from humans. If a female mosquito that bites an infected person, the mosquito may get the dengue virus. At first the virus lives in the cells that line the mosquito's gut. About 8 to 10 days later, the virus spreads to the mosquito's salivary glands, which make saliva (or "spit"). This means that the saliva that the mosquito makes is infected with the dengue virus. So when the mosquito bites a human, its infected saliva goes into the human and can infect that person. The virus does not seem to cause any problems for infected mosquitoes, which will stay infected for the rest of their lives. The Aedes aegypti mosquito is the most likely to spread dengue. This is because it likes to live close to humans and feed off of people instead of animals.[15] It also likes to lay its eggs in man-made water containers.
Dengue can also be spread through infected blood products and through organ donation.[16][17] If a person with dengue donates blood or an organ, which is then given to another person, that person can get dengue from the donated blood or organ. In some countries, like Singapore, dengue is common. In these countries, between 1.6 and 6 blood transfusions out of every 10,000 spread dengue.[18] The dengue virus can also be spread from mother to child during pregnancy or when the child is born.[19] Dengue is usually not spread in any other ways.[7]
Risks
Babies and young children with dengue are more likely than adults to become seriously ill. Children are more likely to become seriously ill if they are well nourished (if they are healthy and well-fed).[5] (This is different from many other infections, which are usually worse in children who are malnourished, not healthy, or not well-fed.) Women are more likely to get seriously ill than men.[20] Dengue can be life-threatening in people with chronic (long-term) diseases, like diabetes and asthma.[20]
Mechanism
When a mosquito bites a person, its saliva enters the person's skin. If the mosquito has dengue, the virus is carried in its saliva. So when the mosquito bites a person, the virus enters the person's skin along with the mosquito saliva. The virus attaches to and enters the person's white blood cells. (The white blood cells are supposed to help defend the body by fighting off threats, like infections.) While the white blood cells move around the body, the virus reproduces (or makes more of itself). The white blood cells react by making many signaling proteins, like interferon. These proteins cause the fever, flu-like symptoms, and severe pains that happen with dengue.
If a person has a severe (serious) infection, the virus reproduces much more quickly inside the body. Because there is a lot more of the virus, it can affect many more organs (like the liver and the bone marrow). Fluid from the bloodstream leaks through the walls of small blood vessels into body cavities. Because of this, less blood circulates (or moves around the body) in the blood vessels. The person's blood pressure becomes so low that the heart cannot supply enough blood to the vital (most important) organs. Also, the bone marrow is not able to make enough platelets, which are needed for the blood to clot correctly. Without enough platelets, the person is much more likely to have bleeding problems. Bleeding is a major complication of dengue (one of the most serious problems that the disease can cause).[21]
Diagnosis
Usually, doctors diagnose dengue by examining the infected person and realizing that his symptoms match dengue. Doctors are especially likely to be able to diagnose dengue this way in areas where it is known to be common.[1] However, when dengue is in its early stages, it can be difficult to tell the difference between this disease and other viral infections (infections caused by viruses).[5] A person probably has dengue if he has a fever and two of these symptoms: nausea and vomiting; a rash; generalized pains (pain all over); a low count (or number) of white blood cells; or a positive tourniquet test. Any warning signs, plus a fever, usually signal that a person has dengue in areas where the disease is common[22].
Warning signs usually show up before dengue becomes severe.[8] The tourniquet test is useful when no laboratory test can be done. To do the tourniquet test, a doctor will wrap a blood pressure cuff around a person's arm for 5 minutes. The doctor will then count any small red spots on the skin. A higher number of spots means that the person is more likely to have dengue fever.[8]
It can be difficult to tell the difference between dengue fever and chikungunya. Chikungunya is a similar viral infection that has many of the same symptoms of dengue, and happens in the same parts of the world.[7] Dengue can also have some of the same symptoms as other diseases, like malaria, leptospirosis, typhoid fever, and meningococcal disease. Often, before a person is diagnosed with dengue, his doctor will do tests to make sure that he does not actually have one of these conditions.[5]
When a person has dengue, the earliest change that can be seen in laboratory tests is a low count (or number) of white blood cells. A low platelet count and metabolic acidosis are also signs of dengue.[5] If the person has severe dengue, there will also be other changes that can be seen if his blood is studied. Severe dengue causes fluid to leak from the bloodstream. This causes hemoconcentration (where there is less plasma - the liquid part of the blood - and more red blood cells in the blood). It also causes low levels of albumin levels in the blood.[5]
Sometimes, severe dengue causes large pleural effusions (where leaked fluid builds up around the lungs) or ascites (where fluid builds up in the abdomen). If these are large enough, a doctor may notice them when he examines the person.[5] A doctor can diagnose dengue shock syndrome early on if he can use a medical ultrasound to find fluid inside the body.[1][5] But in many areas where dengue is common, most doctors and clinics do not have ultrasound machines.[1]
Classification
In 2009, the World Health Organization (WHO) classified, or divided, dengue fever into two types: uncomplicated and severe.[1][22] Before this, in 1997, the WHO had divided the disease into undifferentiated fever, dengue fever, and dengue hemorrhagic fever. The WHO decided that this old way of dividing dengue needed to be made simpler. It also decided that the old way was too restrictive: it did not include all of the ways that dengue can present itself. Although the dengue classification was officially changed, the older classification often is still used.[22][5][23]
In the WHO's old system of classification, dengue hemorrhagic fever was divided into four stages, called grades I–IV:
- In Grade I, the person has a fever. He also bruises easily or has a positive tourniquet test.
- In Grade II, the person bleeds into the skin and other parts of the body.
- In Grade III, the person shows signs of circulatory shock.
- In Grade IV, the person has shock so severe that his blood pressure and heartbeat cannot be felt.[23] Grades III and IV are called "dengue shock syndrome."[22][23]
Laboratory tests
Dengue fever can be diagnosed by microbiological laboratory testing.[22] A few different tests can be done. One test (virus isolation) isolates (or separates out) the dengue virus in cultures (or samples) of cells. Another test (nucleic acid detection) looks for nucleic acids from the virus, using a technique called polymerase chain reaction (PCR). A third test (antigen detection) looks for antigens from the virus. Another test looks in the blood for antibodies which the body makes to fight the dengue virus.[20][24] The virus isolation and nucleic acid detection tests work better than antigen detection. However, these tests cost more, so they are not available in many places.[24] When dengue is in the early stages of the disease, all of these tests may be negative (meaning they do not show that the person has the disease).[5][20]
Except for antibody tests, these laboratory tests can only help diagnose dengue fever during the acute (beginning) stage of the illness. However, antibody tests can confirm that a person has dengue in the later stages of the infection. The body makes antibodies which specifically fight the dengue virus after 5 to 7 days.[7][20][25]
Prevention
There are no vaccines that have been approved to prevent people from getting the dengue virus.[1] To prevent infection, the World Health Organization (WHO) suggests controlling the mosquito population and protecting people from mosquito bites.[13][26]
The WHO suggests a program for preventing dengue (called an "Integrated Vector Control" program) that includes five different parts:
- Advocacy, social mobilization, and legislation (laws) should be used to make public health organizations and communities stronger.
- All parts of society should work together. This includes the public sector (like the government), the private sector (like businesses and corporations), and the health care field.
- All ways of controlling disease should be integrated (or brought together), so that the resources that are available can have the biggest possible effect.
- Decisions should be made based on evidence. This will help make sure that interventions (things that are done to address dengue) are helpful.
- Areas where dengue is a problem should be given help, so that they can build their abilities to respond well to the disease on their own.[13]
The WHO also suggests doing some specific things to control mosquites and keep from getting bitten. The best way to control the “A. aegypti” mosquito is to get rid of its habitats.[13] People should empty out open containers of water (so that mosquitoes cannot lay eggs in them). Insecticides or biological control agents can also be used to control mosquitoes in these areas.[13] Scientists think that spraying with organophosphate or pyrethroid insecticides does not help.[3] Standing water (which does not move) should be gotten rid of, because it attracts mosquitoes, and also because people can have health problems if insecticides build up in standing water.[13] To prevent mosquito bites, people can wear clothing that fully covers their skin. They can use insect repellent (like bug spray), which helps keep mosquitoes away. (DEET works best.) People can also use mosquito netting when they are resting.[14]
Management
There are no specific treatments for dengue fever.[1] Different people need different treatments, depending on their symptoms. Some people can get better just by drinking fluids at home, with their doctor following up closely to make sure they are getting better. Other people need intravenous fluids and blood transfusion.[27] A doctor may decide to admit a person into the hospital if he has serious warning signs, especially if he already has a chronic health condition.[5]
When infected people need intravenous fluids, they usually need them only for a day or two.[27] A doctor will increase the amount of fluid given so that the person gives out a certain amount of urine (0.5–1 mL/kg/hr). The fluid is also increased until the person's hematocrit (the amount of iron in their blood) and their vital signs go back to normal.[5] Because of the risk of bleeding, doctors try to stay away from invasive medical procedures like nasogastric intubation (putting a tube down the person's nose into their stomach), intramuscular injections (giving medicine as a shot into a muscle), and arterial punctures (putting a needle into an artery).[5] Acetaminophen (Tylenol) can be given for fever and pain. A type of anti-inflammatory drug called NSAIDs (like ibuprofen and aspirin) should not be used because they make bleeding more likely.[27] Blood transfusions should be started early if a person's vital signs change or are not normal, and if the amount of red blood cells in their blood is getting lower.[28] When a transfusion is needed, the person should be given whole blood (blood that has not been separated into its different parts) or packed red blood cells. Platelets (separated out from whole blood) and fresh frozen plasma usually are not recommended.[28]
When a person is in the recovery stage of dengue, he usually will not be given any more intravenous fluids so that he doesn't get fluid overload.[5] If fluid overload happens, but the person's vital signs are stable (not changing), it can be enough just to stop giving more fluid.[28] If a person is no longer in the critical stage of the disease, they can be given a loop diuretic such as furosemide (Lasix). This can help get rid of extra fluid from the person's blood circulation.[28]
Likelihood
Most people with dengue recover and don't have any problems afterward.[22] Without treatment, 1 to 5% of infected people 1 to 5 out of every 100) die from dengue.[5] With good treatment, less than 1% die.[22] However, in people with severe dengue, 26% die (26 out of every 100)..[5]
Dengue is common in more than 110 countries.[5] Every year, it infects 50 to 100 million people around the world. It also causes half a million hospitalizations[1] and about 12,500 to 25,000 deaths around the world each year.[6][29]
Dengue is the most common viral disease that is spread by arthropods.[12] Dengue is thought to have a disease burden of about 1600 disability-adjusted life years per million population. This means that in every million people, dengue causes about 1600 years of life to be lost. This is sbout the same disease burden that other childhood and tropical diseases, like tuberculosis, cause.[20] Dengue is thought to be the second most important tropical disease, behind malaria.[5] The World Health Organization also counts dengue as one of 16 neglected tropical diseases (meaning that dengue is not taken as seriously as it should be).[30]
Dengue is becoming much more common around the world. In 2010, dengue was 30 times more common than it was in 1960.[31] Several things are thought to be causing the increase in dengue. More people are living in cities. The world's population (the number of people in the world) is growing. More people are travelling internationally (between countries). Global warming is also thought to play a part in the increase in dengue.[1]
Dengue happens most around the equator. 2.5 billion people live in areas where dengue happens. 70% of these people live in Asia and the Pacific.[31] In the United States, 2.9% to 8% of people who come back from traveling in areas where dengue happens, and have a fever, were infected while traveling.[14] In this group of people, dengue is the second most common infection to be diagnosed, after malaria.[7]
History
Dengue was first written about many years ago. A Chinese medical encyclopedia from the Jin Dynasty (which existed from 265 to 420 AD) talked about a person who probably had dengue. The book talked about a "water poison" that had to do with flying insects.[32][33] There are also written records from the 17th century (the 1600s) about what may have been epidemics of dengue (where the disease spread very quickly in a short time). The most likely early reports of dengue epidemics are from 1779 and 1780. These reports talk about an epidemic that swept Asia, Africa, and North America.[33] From that time until 1940, there were not many more epidemics..[33]
In 1906, scientists proved that people were getting infections from Aedes mosquitoes. In 1907, scientists showed that a virus causes dengue. This was just the second disease that was shown to be caused by a virus. (Scientists had already proven that a virus causes yellow fever.)[34] John Burton Cleland and Joseph Franklin Siler kept studying the dengue virus, and figured out the basics of hoe the virus spreads.[34]
Dengue began to spread much more quickly during and after the Second World War. This is thought to be because the war changed the environment in different ways. Different types of dengue also spread to new areas. For the first time, people started to get dengue hemorrhagic fever. This severe form of the disease was first reported in the Philippines in 1953. By the 1970s, dengue hemorrhagic fever had become a major cause of death in children. It had also started happening in the Pacific and the Americas.[33] Dengue hemorrhagic fever and dengue shock syndrome were first reported in Central and South America in 1981. At this time, doctors noticed that people who had already gotten the type 1 dengue virus were getting type 2 dengue a few years later.[11]
History of the word
It is not clear where the word "dengue" came from. Some people think that it comes from the Swahili phrase Ka-dinga pepo. This phrase talks about the disease being caused by an evil spirit.[32] The Swahili word dinga is thought to come from the Spanish word dengue. This word means "careful". That word may have been used to describe a person suffering from the bone pain of dengue fever; that pain would make the person walk carefully.[35] However, it is also possible that the Spanish word came from the Swahili word, and not the other way around.[32]
Other people think that the name "dengue" comes from the West Indies. In the West Indies, slaves that had dengue were said to stand and walk like "a dandy". Because of this, the disease was also called "dandy fever."[36][37]
The name "breakbone fever" was first used by Benjamin Rush, a doctor and United States "Founding Father". In 1789, Rush used the name "breakbone fever" in a report about the 1780 dengue outbreak in Philadelphia. In the report, Rush mostly used the more formal name "bilious remitting fever".[38][39] The term "dengue fever" was not commonly used until after 1828.[37] Before that, different people used different names for the disease. For example, dengue was also called "breakheart fever" and "la dengue."[37] Other names were also used for severe dengue: for example, "infectious thrombocytopenic purpura", "Philippine," "Thai," and "Singapore hemorrhagic fever."[37]
Research
Scientists keep doing research on ways to prevent and treat dengue. People are also working on controlling mosquitoes,[40] creating a vaccine, and creating drugs to fight the virus.[26]
Many simple things have been done to control mosquitoes. Some of these things have worked. For example, guppies (Poecilia reticulata) or copepods can be put in standing water to eat the mosquito larvae (eggs).[40]
Scientists keep working on creating a vaccine to protect people from all four types of dengue.[26] Some scientists worry that a vaccine could increase the risk of severe disease through antibody-dependent enhancement (ADE).[41] The best possible vaccine would have a few different qualities. First, it would be safe. Second, it would work after one or two injections (or shots). Third, it would protect against all types of the dengue virus. Fourth, it would not cause ADE. Fifth, it would be easy to transport (move) and store (keep until it is needed). Sixth, it would be low-cost and be cost-effective (worth the cost).[41] A few vaccines had been tested by 2009.[20][38][41] Scientists hope that the first vaccine (or vaccines) will be commercially available (available to buy) by 2015.[26]
Scientists also keep working on creating antiviral drugs to treat attacks of dengue fever and keep people from getting severe complications.[42][43] They are also working on figuring out how the virus's proteins are structured. This may help them create medications that work well for dengue.[43]
Notes
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Whitehorn J, Farrar J (2010). "Dengue". Br. Med. Bull. 95: 161–73. doi:10.1093/bmb/ldq019. PMID 20616106.
- ↑ 2.0 2.1 2.2 WHO (2009), pp. 14–16.
- ↑ 3.0 3.1 3.2 Reiter P (2010-03-11). "Yellow fever and dengue: a threat to Europe?". Euro Surveil. 15 (10): 19509. PMID 20403310.
- ↑ Gubler (2010), p. 379.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 5.19 5.20 5.21 5.22 5.23 5.24 5.25 5.26 Ranjit S, Kissoon N (2010). "Dengue hemorrhagic fever and shock syndromes". Pediatr. Crit. Care Med. 12 (1): 90–100. doi:10.1097/PCC.0b013e3181e911a7. PMID 20639791.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 6.0 6.1 6.2 6.3 6.4 Varatharaj A (2010). "Encephalitis in the clinical spectrum of dengue infection". Neurol. India. 58 (4): 585–91. doi:10.4103/0028-3886.68655. PMID 20739797.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Chen LH, Wilson ME (2010). "Dengue and chikungunya infections in travelers". Curr. Opin. Infect. Dis. 23 (5): 438–44. doi:10.1097/QCO.0b013e32833c1d16. PMID 20581669.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 WHO (2009), pp. 25–27.
- ↑ 9.0 9.1 Wolff K, Johnson RA (eds.) (2009). "Viral Infections of Skin and Mucosa". Fitzpatrick's Color Atlas and Synopsis of Clinical Dermatology (6th ed.). New York: McGraw-Hill Medical. pp. 810–2. ISBN 9780071599757.
{{cite book}}:|author=has generic name (help) - ↑ 10.0 10.1 Knoop KJ, Stack LB, Storrow A, Thurman RJ (eds.) (2010). "Tropical Medicine". Atlas of Emergency Medicine (3rd ed.). New York: McGraw-Hill Professional. pp. 658–9. ISBN 0071496181.
{{cite book}}:|author=has generic name (help)CS1 maint: multiple names: authors list (link) - ↑ 11.0 11.1 11.2 11.3 11.4 Gould EA, Solomon T (2008). "Pathogenic flaviviruses". The Lancet. 371 (9611): 500–9. doi:10.1016/S0140-6736(08)60238-X. PMID 18262042.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 12.0 12.1 Rodenhuis-Zybert IA, Wilschut J, Smit JM (2010). "Dengue virus life cycle: viral and host factors modulating infectivity". Cell. Mol. Life Sci. 67 (16): 2773–86. doi:10.1007/s00018-010-0357-z. PMID 20372965.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 13.0 13.1 13.2 13.3 13.4 13.5 WHO (2009), pp. 59–60.
- ↑ 14.0 14.1 14.2 Center for Disease Control and Prevention. "Chapter 5 – Dengue Fever (DF) and Dengue Hemorrhagic Fever (DHF)". 2010 Yellow Book. Retrieved 2010-12-23.
- ↑ Gubler (2010), pp. 377–78.
- ↑ Wilder-Smith A, Chen LH, Massad E, Wilson ME (2009). "Threat of Dengue to Blood Safety in Dengue-Endemic Countries". Emerg. Infect. Dis. 15 (1): 8–11. doi:10.3201/eid1501.071097. PMC 2660677. PMID 19116042.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Stramer SL, Hollinger FB, Katz LM; et al. (2009). "Emerging infectious disease agents and their potential threat to transfusion safety". Transfusion. 49 Suppl 2: 1S–29S. doi:10.1111/j.1537-2995.2009.02279.x. PMID 19686562.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Teo D, Ng LC, Lam S (2009). "Is dengue a threat to the blood supply?". Transfus Med. 19 (2): 66–77. doi:10.1111/j.1365-3148.2009.00916.x. PMC 2713854. PMID 19392949.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Wiwanitkit V (2010). "Unusual mode of transmission of dengue". Journal of Infection in Developing Countries. 4 (1): 51–4. PMID 20130380.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 Guzman MG, Halstead SB, Artsob H; et al. (2010). "Dengue: a continuing global threat". Nat. Rev. Microbiol. 8 (12 Suppl): S7–S16. doi:10.1038/nrmicro2460. PMID 21079655.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Martina BE, Koraka P, Osterhaus AD (2009). "Dengue Virus Pathogenesis: an Integrated View". Clin. Microbiol. Rev. 22 (4): 564–81. doi:10.1128/CMR.00035-09. PMC 2772360. PMID 19822889.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 WHO (2009), pp. 10–11.
- ↑ 23.0 23.1 23.2 WHO (1997). "Chapter 2: clinical diagnosis". Dengue haemorrhagic fever: diagnosis, treatment, prevention and control (PDF) (2nd ed.). Geneva: World Health Organization. pp. 12–23. ISBN 9241545003.
- ↑ 24.0 24.1 WHO (2009), pp. 90–95.
- ↑ Gubler (2010), p. 380.
- ↑ 26.0 26.1 26.2 26.3 WHO (2009), p. 137. Cite error: Invalid
<ref>tag; name "WHOp137" defined multiple times with different content - ↑ 27.0 27.1 27.2 WHO (2009), pp. 32–37.
- ↑ 28.0 28.1 28.2 28.3 WHO (2009), pp. 40–43.
- ↑ WHO media centre (March 2009). "Dengue and dengue haemorrhagic fever". World Health Organization. Retrieved 2010-12-27.
- ↑ Neglected Tropical Diseases. "Diseases covered by NTD Department". World Health Organization. Retrieved 2010-12-27.
- ↑ 31.0 31.1 WHO (2009), p. 3.
- ↑ 32.0 32.1 32.2 Anonymous (2006). "Etymologia: dengue" (PDF). Emerg. Infec. Dis. 12 (6): 893.
- ↑ 33.0 33.1 33.2 33.3 Gubler DJ (1998). "Dengue and Dengue Hemorrhagic Fever". Clin. Microbiol. Rev. 11 (3): 480–96. PMC 88892. PMID 9665979.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 34.0 34.1 Henchal EA, Putnak JR (1990). "The dengue viruses". Clin. Microbiol. Rev. 3 (4): 376–96. doi:10.1128/CMR.3.4.376. PMC 358169. PMID 2224837.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Harper D (2001). "Etymology: dengue". Online Etymology Dictionary. Retrieved 2008-10-05.
- ↑ Anonymous (1998-06-15). "Definition of Dandy fever". MedicineNet.com. Retrieved 2010-12-25.
- ↑ 37.0 37.1 37.2 37.3 Halstead SB (2008). Dengue (Tropical Medicine: Science and Practice). River Edge, N.J: Imperial College Press. pp. 1–10. ISBN 1-84816-228-6.
- ↑ 38.0 38.1 Barrett AD, Stanberry LR (2009). Vaccines for biodefense and emerging and neglected diseases. San Diego: Academic. pp. 287–323. ISBN 0-12-369408-6.
- ↑ Rush AB (1789). "An account of the bilious remitting fever, as it appeared in Philadelphia in the summer and autumn of the year 1780". Medical enquiries and observations. Philadelphia: Prichard and Hall. pp. 104–117.
- ↑ 40.0 40.1 WHO (2009), p. 71.
- ↑ 41.0 41.1 41.2 Webster DP, Farrar J, Rowland-Jones S (2009). "Progress towards a dengue vaccine". Lancet Infect Dis. 9 (11): 678–87. doi:10.1016/S1473-3099(09)70254-3. PMID 19850226.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Sampath A, Padmanabhan R (2009). "Molecular targets for flavivirus drug discovery". Antiviral Res. 81 (1): 6–15. doi:10.1016/j.antiviral.2008.08.004. PMC 2647018. PMID 18796313.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 43.0 43.1 Noble CG, Chen YL, Dong H; et al. (2010). "Strategies for development of Dengue virus inhibitors". Antiviral Res. 85 (3): 450–62. doi:10.1016/j.antiviral.2009.12.011. PMID 20060421.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
References
- Gubler DJ (2010). "Dengue viruses". In Mahy BWJ, Van Regenmortel MHV (ed.). Desk Encyclopedia of Human and Medical Virology. Boston: Academic Press. pp. 372–82. ISBN 0-12-375147-0.
- WHO (2009). Dengue Guidelines for Diagnosis, Treatment, Prevention and Control (PDF). Geneva: World Health Organization. ISBN 9241547871.
