Syphilis
| Syphilis | |
|---|---|
| Classification and external resources | |
 Treponema pallidum bacteria under an electron microscope | |
| ICD-10 | A50.-A53. |
| ICD-9 | 090-097 |
| DiseasesDB | 29054 |
| MedlinePlus | 001327 |
| eMedicine | med/2224 emerg/563 derm/413 |
| MeSH | D013587 |
Syphilis is a sexually transmitted infection caused by a bacterium called Treponema pallidum. Syphilis is usually spread by sexual contact. However, a fetus can get syphilis from its mother while she is pregnant or during childbirth. This is called congenital syphilis.
There are four stages of syphilis: the primary, secondary, latent, and tertiary stages. In each stage, the signs and symptoms of syphilis are different.
In the primary stage, a person usually just has a wound on their skin, called a "chancre." In the secondary stage, a person usually gets a rash. In the "latent" stage, syphilis has few or no symptoms. If syphilis reaches the tertiary stage, which is the most severe, it causes many serious symptoms. These can include problems with the nervous system (the brain and nerves) and problems with the heart. Many people with tertiary syphilis will die if they do not get medical treatment.
Syphilis is usually diagnosed with blood tests. The bacteria that causes syphilis can also be seen under a microscope. Most people who have syphilis can be treated and cured with antibiotics.
By 1999, more than 12 million people around the world had syphilis. More than 90% of these people (10.8 million) lived in the developing world.[1] Syphilis got much less common after penicillin became available in the 1940s. At that time, penicillin was used as a treatment for syphilis, and often cured the disease. Since 2000, syphilis is becoming more common again.[1]
Syphilis is a very dangerous disease if it is not treated. Without treatment, 8% to 58% of people with syphilis die from the disease. Syphilis also makes a person two to five times more likely to get Human Immunodeficiency Virus (HIV).[1][2]
Stages of syphilis[change | change source]
Primary stage[change | change source]

When a person gets syphilis, the disease is in the primary stage. A person gets syphilis by having sex with a person who has syphilis. Usually, the person who has syphilis has infectious lesions on their genitals caused by syphilis. Touching or kissing these wounds during sex (including oral sex or anal sex) can give a person syphilis.[3]
Later, a chancre (skin sore) usually appears at the place on the body that touched the infected wounds.[2] The chancre can be painful. The most common type of chancre gets bigger and bigger until it becomes an ulcer.[4]
Chancres can appear in places other than the genitals. In women, chancres most often appear on the cervix - the bottom of the uterus. Some people get no chancres at all. Many people who have secondary syphilis (40–85% of women and 20–65% of men) say they never had a chancre during the primary stage.[5]
Around the place where syphilis entered the body, the lymph nodes usually get bigger[2] about 7 to 10 days after the chancre forms.[4] If the person does not get treatment, their wound(s) can last for three to six weeks.[2]
Secondary stage[change | change source]

If a person does not get treatment, syphilis will get worse. The secondary stage of syphilis will start about four to ten weeks after the person first got infected.[2] Secondary syphilis can cause many different symptoms. The most common three symptoms are:[5]
- Sores on the mucous membranes (like the nose, throat, genitals, or anus)[5]
- A rash on the chest, back, hands, and/or feet
- Swollen lymph nodes
All of the sores that people get during this stage can spread syphilis. The bacteria lives inside the wounds.[2][6]
The symptoms of secondary syphilis usually get better after three to six weeks.[7] However, in about 25% of cases (1 out of every 4), these symptoms return.
Latent stage[change | change source]
In the latent stage of syphilis, a person has no symptoms, but blood tests show that he has syphilis.[3] Latent syphilis is described as either early or late.
- The early latent stage: In the United States, latent syphilis is called "early" if it has been less than one year since the person had secondary syphilis.[7] In the United Kingdom, latent syphilis is called "early" if it has been less than two years.[4] In this stage, the symptoms of secondary syphilis can still come back.
- The late latent stage: People enter this stage when it has been more than one year (in the U.S.) or more than two years (in the U.K.) since they had secondary syphilis. People in this stage have no symptoms, and do not spread syphilis as easily as people in the early latent stage.[7]
Tertiary stage[change | change source]

If a person with syphilis does not get treatment, the disease can reach the worst stage - tertiary syphilis. Usually this happens about three to 15 years after the person first got infected. Without treatment, one-third of people with syphilis get tertiary disease.[7] People with tertiary syphilis cannot infect other people with syphilis.[2]
There are three different forms of tertiary syphilis.
Gummatous syphilis (late benign syphilis)[change | change source]
Gummatous syphilis can happen anywhere from one to 46 years after the person first got syphilis. On average, it happens after 15 years. It causes soft, tumor-like balls of inflammation (swelling), of many different sizes. Usually they appear on the skin, bone, and liver, but they can happen anywhere.
About 15% of people who do not get treated for syphilis get gummatous syphilis.
Neurosyphilis[change | change source]

In neurosyphilis, the syphilis infects the central nervous system (the brain and spinal cord). In some people, neurosyphilis happens soon after they get syphilis. (This is called early neurosyphilis.) Some of these people have no symptoms of neurosyphilis. Others get syphilitic meningitis, a dangerous infection of the meninges (the protective layers which line the brain and spinal cord).
Neurosyphilis can also appear later, usually four to 25 years after a person first got syphilis. (This is called late neurosyphilis.) Late neurosyphilis can cause many serious problems. For example:
- Meningovascular syphilis, which causes seizures
- General Paresis: In this brain disease, syphilis causes chronic meningoencephalitis - an infection of both the meninges and the brain which does not go away. This causes parts of the brain to die.[2]
- Because of this, the person gets dementia (which causes problems with the way a person thinks, remembers, acts, and behaves toward other people)
- The person also gets tabes dorsalis (which causes problems with balance, and pain in the legs and feet)
About 6.5% of people who do not get treated for syphilis get late neurosyphilis.
Cardiovascular syphilis[change | change source]
This type of tertiary syphilis causes problems with the cardiovascular system (the heart and blood vessels). It usually happens 10 to 30 years after the person first got infected with syphilis. The most common problem it causes is syphilitic aortitis, which affects the aorta. The aorta is the most important artery in the heart; it helps carry blood to the entire body. Syphilitic aortitis can make the aorta become too big.[2] If the aorta is too big, it cannot work correctly.
About 10% of people who do not get treated for syphilis get cardiovascular syphilis.
Congenital syphilis[change | change source]
Congenital syphilis is spread from a mother to her fetus during pregnancy or childbirth.
Two out of every three infants born with syphilis have no symptoms. In the other infants, symptoms can appear as the baby gets older. The most common symptoms are:[8]
- Hepatosplenomegaly (where two important organs, the liver and spleen, are larger than usual)
- Rash
- Fever
- Neurosyphilis
- Swelling in the lungs
If babies with syphilis do not get treated, they can get late congenital syphilis, which has much more serious symptoms. For example, the child can have seizures, and their body and brain may not grow normally.[8]
Cause[change | change source]
Bacteria[change | change source]

Syphilis is caused by the Treponema pallidum bacterium. Treponema pallidum is a species of bacterium which is shaped like a spiral: a spirochaete.[9] There are different types of Treponema pallidum bacteria, which are called subspecies.[8]
Scientists think that Treponema pallidum can only live inside humans.[1] The bacterium cannot survive outside a human for more than a few days.
Transmission: how syphilis is spread[change | change source]
Syphilis is spread mostly by sexual contact or during pregnancy from a mother to her fetus. Syphilis can pass through undamaged mucous membranes, or through damaged skin.[1][2] Because of this, syphilis can be spread through oral sex, vaginal sex, and anal sex.[2] It can also be spread by kissing, if the person with syphilis has a sore in their mouth.[2]
Only a very small amount of the Treponema pallidum bacterium needs to get into a person's body to cause syphilis. Not everybody who is exposed to primary or secondary syphilis will get the disease.[7]
A person can get syphilis if they get a blood transfusion from someone with the disease. However, many countries test blood donations for syphilis. In countries that do not do this, getting syphilis from a blood transfusion is much more likely.
Scientists think syphilis is usually not spread by sharing needles[2] (using the same needles to inject drugs).
A person cannot get syphilis from sitting on a toilet seat; using a hot tub or a swimming pool; sharing plates, cups, or utensils; sharing clothing; or doing other regular daily activities.[10]
Diagnosis[change | change source]

It is hard for doctors to diagnose syphilis just from the signs and symptoms that happen early on, because many diseases can cause skin sores and rashes.[4] Instead, they can diagnose syphilis by doing a blood test, or by looking at the blood under a microscope. Blood tests are used more often, because they are easier to do. However, blood tests cannot tell which stage of syphilis a person has.
Prevention[change | change source]
As of 2010[update], there is no vaccine that prevents syphilis.[1]
Safer sex[change | change source]
Not having sexual contact with a person who has syphilis is the best way to prevent getting syphilis.
If a person does not know if their sexual partner has syphilis, having safer sex can help protect them. For example, using a latex condom the right way lowers the risk of getting a sexually transmitted disease like syphilis. However, even if a person uses a condom, it is still possible to get syphilis.[10][11]
The United States Centers for Disease Control and Prevention (CDC) says that the best ways to prevent syphilis are:[10]
- To be in a long-term relationship with a partner who does not have syphilis;
- For both partners to be loyal in their relationship and not have sexual contact with anyone else; and
- To avoid using alcohol or other drugs, because they make people more likely to have risky, unsafe sex, which can spread syphilis.
Preventing congenital syphilis[change | change source]
Congenital syphilis in newborn babies can be prevented by testing mothers for syphilis during early pregnancy and treating women who are infected.[12] By doing this in 2015, Cuba became the first country in the world to eradicate the spread of syphilis from Cuban mothers to their babies.
The United States Preventive Services Task Force [13] and the World Health Organization[14] say that all pregnant women should be tested for syphilis. If a woman tests positive, her sexual partners (the people she has had sex with) should also be treated.[14]
In most developed countries, congenital syphilis is not common. It still happens once in a while, when women do not get any health care during pregnancy.[12] However, congenital syphilis is much more common in developing countries. Many women in these countries do not get healthcare during pregnancy, and others get healthcare that does not include testing for syphilis.[12] When there are programs that make syphilis testing easier to get, fewer babies get congenital syphilis in these countries.[14]
Preventing syphilis from spreading[change | change source]
The CDC says that men who have sex with men should be tested at least every year.[15] Getting tested regularly helps prevent syphilis from being spread. If a person is tested and finds out that they have syphilis, they are more likely to get treatment, and will not accidentally spread syphilis to other people.
Syphilis is a notifiable disease in many places, including Canada,[16] the countries in the European Union,[17] and the United States.[18] This means that if a healthcare provider (like a doctor or a nurse) knows that a patient has syphilis, they must tell public health authorities that the patient is infected. Public health workers then talk to all of the patient's sexual partners. They tell them someone might have given them syphilis, without telling them who that person is.[19] Doctors might also try to get patients with syphilis to tell their sexual partners to get treatment.[20]
Treatment[change | change source]

Early infections[change | change source]
Syphilis that is not complicated can usually be treated and cured by antibiotic medications.
Usually, people need just one dose of penicillin G or azithromycin.[21] If a person cannot take either of these medicines (for example, because they are allergic to them), some other medications work too. For example, Doxycycline and tetracycline are two other possible choices; however, they cannot be used in pregnant women.
The Treponema pallidum bacterium has become resistant to many different antibiotics, including macrolides, clindamycin, and rifampin.[1] These antibiotics no longer kill the bacterium.
Late infections[change | change source]
Once a person is in the later stages of syphilis, the disease is harder to treat.
For example, if a person has neurosyphilis, they need antibiotics that will kill the infection in their central nervous system (their brain and major nerves). It is hard for penicillin G to get into the central nervous system. Because of this, a single shot of penicillin - which will usually cure early syphilis - is not enough to cure neurosyphilis. Instead, people with neurosyphilis usually need to be given large doses of penicillin for at least 10 days. Usually, they also need to get the medicine intravenously (through a needle placed into a vein) so it goes more directly to the central nervous system.[1][2] If a person is allergic to penicillin, other antibiotics like ceftriaxone, doxycycline, or tetracycline can be used, but they have to be given over longer periods of time.[2]
Once a person has late-stage syphilis, treatment will keep their syphilis from getting any worse. However, if syphilis has already damaged the person's body, the treatment will not make that damage go away. At best, treatment can only have a very small effect on the damage that has already happened.[2]
Jarisch-Herxheimer reaction[change | change source]
Sometimes, the treatment for syphilis can cause a side effect called the Jarisch-Herxheimer reaction. This usually starts within one hour after treatment begins, and lasts for 24 hours. Its symptoms include fever, muscle pains, headache, and a fast heart rate.[2] Antibiotic medication breaks open syphilis bacteria to kill them. As the bacteria break open, proteins come out of them. These proteins cause the Jarisch-Herxheimer reaction.[22]
Epidemiology[change | change source]
In 1999, syphilis had infected about 12 million people. More than 90% of these people lived in the developing world.[1]

Syphilis causes problems in 700,000 to 1.6 million pregnancies every year. Syphilis can cause a pregnant woman to have a miscarriage, a stillbirth, a premature baby, a baby with congenital syphilis, or a baby that dies before it is a month old.[8] In sub-Saharan Africa, syphilis causes up to 20% of perinatal deaths (deaths that happen soon after a baby is born).[8]
Syphilis used to be very common, and it caused sickness and death all over the world. It was very common in Europe during the 18th and 19th centuries. During the early 20th century, syphilis became less common in the developed world, because antibiotics were being used more and more. Syphilis kept becoming less common until the 1980s and 1990s.[9] Since the year 2000, syphilis is getting more common again in the United States, the United Kingdom, Australia, and Europe, mostly among men who have sex with men.[1]
In China and Russia, syphilis has become more common among heterosexual people since the 1990s.[1] Studies say this is because of unsafe sexual practices, like having sex with many different people, prostitution (getting paid to have sex), and not having safer sex to protect against sexually transmitted diseases.[1][24][25]
Over the 19th and 20th centuries, the symptoms of syphilis have become less severe (not quite as bad). This is partly because there are more treatments that work well, and if they are given early, syphilis does not get as bad. Also, the bacteria that causes syphilis has become weaker.[5]
If people with syphilis get treated early on, they can usually be cured without the disease causing damage that cannot be fixed.[4] Syphilis still causes serious problems, and sometimes death, if it is not treated. Syphilis also makes a person two to five times more likely to get HIV. Confection (having both syphilis and HIV) is common. In some big cities, it happens in as many as 30% to 60% of people with syphilis.[1][2]
History[change | change source]
Nobody knows exactly where and how syphilis started.[2] There are two major ideas about where the disease came from.
The first idea is called the "Columbian hypothesis." (A hypothesis is an educated guess about how something happened). This hypothesis says that when Christopher Columbus's crew came back to Europe after exploring the "New World", they brought syphilis back to Europe and spread the disease there.
The other idea is called the "pre-Columbian hypothesis." ("Pre-Columbian" means "before Columbus.") This hypothesis says that syphilis was already in Europe before Columbus, and people just did not realize that the disease existed.[26]
While there is evidence that can be used to say that either of these ideas are right, there is more evidence for the Columbian hypothesis.[27]
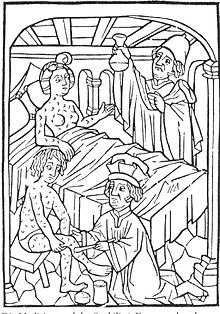
The first written records that talk about an outbreak of syphilis in Europe are from 1494 to 1495. The outbreak happened in Naples, Italy, when France was invading (trying to take over Italy).[9][26] Because syphilis was spread by French soldiers who were coming back from Italy, at first it was called the "French disease."
The name "syphilis" was first used in 1530 by an Italian doctor and poet named Girolamo Fracastoreo. He used the word "syphilis" as the title of a Latin poem that talked about the damage the disease was causing in Italy.[28] At other times in history, syphilis was also called the "Great Pox".[29][30]
In 1905 Fritz Schaudinn and Erich Hoffmann discovered that syphilis is caused by the Treponema pallidum bacteria.[9] Five years later, Paul Ehrlich created the first treatment that helped treat syphilis (called Salvarsan). After that, scientists started to study penicillin. In 1943, it was decided that penicillin worked for syphilis.[9][29] This was a major success in the treatment of syphilis. Before penicillin, the treatments used for syphilis were often even worse than the disease. For example, people were treated with mercury (which is poisonous and causes serious health problems), or people were just kept away from everyone else.[29]
From 1932 to 1972, the United States Public Health Service did a study on syphilis in Alabama. They wanted to see how syphilis got worse when it was not treated. The researchers chose a group of poor African-American sharecroppers, but never told them they had syphilis. Even after the 1940s, when the researchers knew penicillin could cure these people, they refused to let them get treatment or even tell them that penicillin could help them. This study, now called the Tuskegee syphilis experiment, was very important in creating medical ethics.
Many famous people in history may have had syphilis. For example, some people think that Franz Schubert, Arthur Schopenhauer, Édouard Manet,[9] and Adolf Hitler had the disease.[31]
Related pages[change | change source]
References[change | change source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Stamm LV (February 2010). "Global Challenge of Antibiotic-Resistant Treponema pallidum" (PDF). Antimicrob. Agents Chemother. 54 (2): 583–9. doi:10.1128/AAC.01095-09. PMC 2812177. PMID 19805553. Archived from the original (PDF) on 2014-04-25. Retrieved 2012-04-13.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 Kent M.E. & Romanelli F. 2008. Reexamining syphilis: an update on epidemiology, clinical manifestations, and management. Ann Pharmacother 42 (2): 226–36. [1] Archived 2012-10-19 at the Wayback Machine
- ↑ 3.0 3.1 Committee on Infectious Diseases (2006). Larry K. Pickering (ed.). Red book 2006 Report of the Committee on Infectious Diseases (27th ed.). Elk Grove Village, IL: American Academy of Pediatrics. pp. 631–44. ISBN 9781581102079.
- ↑ 4.0 4.1 4.2 4.3 4.4 Eccleston, K; Collins L; Higgins SP (Mar 2008). "Primary syphilis". International Journal of STD & AIDS. 19 (3): 145–51. doi:10.1258/ijsa.2007.007258. PMID 18397550. S2CID 19931104.
- ↑ 5.0 5.1 5.2 5.3 Mullooly, C; Higgins, SP (Aug 2010). "Secondary syphilis: the classical triad of skin rash, mucosal ulceration and lymphadenopathy". International Journal of STD & AIDS. 21 (8): 537–45. doi:10.1258/ijsa.2010.010243. PMID 20975084. S2CID 207198662.
- ↑ Dylewski J, Duong M (2 January 2007). "The rash of secondary syphilis". Canadian Medical Association Journal. 176 (1): 33–5. doi:10.1503/cmaj.060665. PMC 1764588. PMID 17200385.
- ↑ 7.0 7.1 7.2 7.3 7.4 Bhatti MT (2007). "Optic neuropathy from viruses and spirochetes". Int Ophthalmol Clin. 47 (4): 37–66, ix. doi:10.1097/IIO.0b013e318157202d. PMID 18049280. S2CID 2011299.
- ↑ 8.0 8.1 8.2 8.3 8.4 Woods CR (June 2009). "Congenital syphilis-persisting pestilence". Pediatr. Infect. Dis. J. 28 (6): 536–7. doi:10.1097/INF.0b013e3181ac8a69. PMID 19483520.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Franzen, C (Dec 2008). "Syphilis in composers and musicians--Mozart, Beethoven, Paganini, Schubert, Schumann, Smetana". European Journal of Clinical Microbiology and Infectious Diseases. 27 (12): 1151–7. doi:10.1007/s10096-008-0571-x. PMID 18592279. S2CID 947291.
- ↑ 10.0 10.1 10.2 "Syphilis - CDC Fact Sheet". Centers for Disease Control and Prevention (CDC). 16 September 2010. Retrieved 2007-05-30.
- ↑ Koss, Catherine A.; Dunne, Eileen F.; Warner, Lee (July 2009). "A Systematic Review of Epidemiologic Studies Assessing Condom Use and Risk of Syphilis". Sexually Transmitted Diseases. 36 (7): 401–405. doi:10.1097/OLQ.0b013e3181a396eb. ISSN 0148-5717. PMID 19455075. S2CID 25571961.
- ↑ 12.0 12.1 12.2 Schmid, G (Jun 2004). "Economic and programmatic aspects of congenital syphilis prevention". Bulletin of the World Health Organization. 82 (6): 402–9. PMC 2622861. PMID 15356931.
- ↑ U.S. Preventive Services Task, Force (May 19, 2009). "Screening for syphilis infection in pregnancy: U.S. Preventive Services Task Force reaffirmation recommendation statement". Annals of Internal Medicine. 150 (10): 705–9. doi:10.7326/0003-4819-150-10-200905190-00008. PMID 19451577.
- ↑ 14.0 14.1 14.2 Hawkes, Sarah; Matin, Nashaba; Broutet, Nathalie; Low, Nicola (Jun 15, 2011). "Effectiveness of interventions to improve screening for syphilis in pregnancy: a systematic review and meta-analysis". The Lancet Infectious Diseases. 11 (9): 684–91. doi:10.1016/S1473-3099(11)70104-9. PMID 21683653.
- ↑ "Trends in Sexually Transmitted Diseases in the United States: 2009 National Data for Gonorrhea, Chlamydia and Syphilis". Centers for Disease Control and Prevention (CDC). 22 November 2010. Retrieved 3 August 2011.
- ↑ "National Notifiable Diseases". Public Health Agency of Canada. 2005-04-05. Archived from the original on 2011-08-09. Retrieved 2 August 2011.
- ↑ Viñals-Iglesias, H; Chimenos-Küstner, E (Sep 1, 2009). "The reappearance of a forgotten disease in the oral cavity: syphilis". Medicina Oral, Patologia Oral y Cirugia Bucal. 14 (9): e416–20. PMID 19415060.
- ↑ "Table 6.5. Infectious Diseases Designated as Notifiable at the National Level-United States, 2009 [a]". Red Book. Retrieved 2 August 2011.
- ↑ Brunner & Suddarth's textbook of medical-surgical nursing (12th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. 2010. p. 2144. ISBN 9780781785891.
- ↑ Hogben, M (Apr 1, 2007). "Partner notification for sexually transmitted diseases". Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 44 (Suppl 3): S160–74. doi:10.1086/511429. PMID 17342669.
- ↑ Gilbert, David N.; Chambers, Henry F.; Eliopoulos, Georges M.; Saag, Michael S. (2015). The Sanford guide to antimicrobial therapy 2015 (45th ed.). Sperryville, Va. ISBN 978-1-930808-84-3. OCLC 900438957.
{{cite book}}: CS1 maint: location missing publisher (link) - ↑ Pathogenic treponema : molecular and cellular biology. Wymondham, Norfolk, England: Caister Academic. 2006. ISBN 978-1-904455-10-3. OCLC 67375507.
- ↑ The Metropolitan Museum of Art Bulletin, Summer 2007, pp. 55–56.
- ↑ Kent, ME; Romanelli, F (Feb 2008). "Reexamining syphilis: an update on epidemiology, clinical manifestations, and management". The Annals of Pharmacotherapy. 42 (2): 226–36. doi:10.1345/aph.1K086. PMID 18212261. S2CID 23899851.
- ↑ Ficarra, G; Carlos, R (Sep 2009). "Syphilis: The Renaissance of an Old Disease with Oral Implications". Head and Neck Pathology. 3 (3): 195–206. doi:10.1007/s12105-009-0127-0. PMC 2811633. PMID 20596972.
- ↑ 26.0 26.1 Farhi, D; Dupin, N (Sep–Oct 2010). "Origins of syphilis and management in the immunocompetent patient: facts and controversies". Clinics in Dermatology. 28 (5): 533–8. doi:10.1016/j.clindermatol.2010.03.011. PMID 20797514.
- ↑ Rothschild, BM (2005-05-15). "History of syphilis". Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 40 (10): 1454–63. doi:10.1086/429626. PMID 15844068. S2CID 6000907.
- ↑ Nancy G. "Siraisi, Drugs and Diseases: New World Biology and Old World Learning," in Anthony Grafton, Nancy G. Siraisi, with April Shelton, eds., New World, Ancient Texts (Cambridge MA: Belknap Press/Harvard University Press, 1992), 159-94
- ↑ 29.0 29.1 29.2 Dayan, L; Ooi, C (Oct 2005). "Syphilis treatment: old and new". Expert Opinion on Pharmacotherapy. 6 (13): 2271–80. doi:10.1517/14656566.6.13.2271. PMID 16218887. S2CID 6868863.
- ↑ Knell, RJ (2004-05-07). "Syphilis in renaissance Europe: rapid evolution of an introduced sexually transmitted disease?" (PDF). Proceedings. Biological Sciences / The Royal Society. 271 (Suppl 4): S174–6. doi:10.1098/rsbl.2003.0131. PMC 1810019. PMID 15252975.
- ↑ "Hitler syphilis theory revived". BBC News. 12 March 2003.


